Haemorrhoids (Piles)
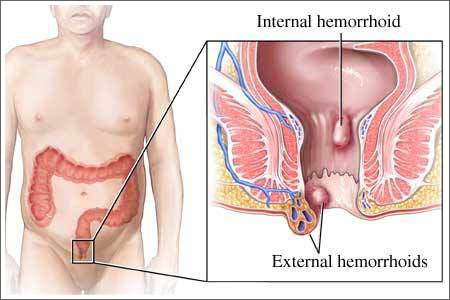
Hemorrhoids, emerods, or piles are swelling and inflammation of
veins in the rectum and anus. The anatomical term "hemorrhoids"
technically refers to "'Cushions of tissue filled with blood vessels at
the junction of the rectum and the anus." However, the term is popularly
used to refer to varicosities of the hemorrhoid tissue. Perianal
hematoma are sometimes misdiagnosed and mislabeled as hemorrhoids, when
in fact they have different causes and treatments.
- External hemorrhoids are those that occur outside the anal
verge (the distal end of the anal canal). Specifically they are
varicosities of the veins draining the territory of the inferior rectal
arteries, which are branches of the pudendal artery. They are sometimes
painful, and can be accompanied by swelling and irritation. Itching,
although often thought to be a symptom of external hemorrhoids, is more
commonly due to skin irritation.
- External hemorrhoids are prone to thrombosis: if the vein
ruptures and/or a blood clot develops, the hemorrhoid becomes a
thrombosed hemorrhoid.
- Internal hemorrhoids are those that occur inside the rectum.
Specifically they are varicosities of veins draining the territory of
branches of the superior rectal arteries. As this area lacks pain
receptors, internal hemorrhoids are usually not painful and most people
are not aware that they have them. Internal hemorrhoids, however, may
bleed when irritated, usually due to constipation.
- Untreated internal hemorrhoids can lead to two severe forms of hemorrhoids: prolapsed and strangulated hemorrhoids:
- Prolapsed hemorrhoids are internal hemorrhoids that are so distended that they are pushed outside the anus.
- If the anal sphincter muscle goes into spasm and traps a
prolapsed hemorrhoid outside the anal opening, the supply of blood is
cut off, and the hemorrhoid becomes a strangulated hemorrhoid.
Classification by degree of prolapse:
The most common grading system was developed by Banov:
Grading of Internal Hemorrhoids
- Grade I: The hemorrhoids do not prolapse.
- Grade II: The hemorrhoids prolapse upon defecation but spontaneously reduce.
- Grade III: The hemorrhoids prolapse upon defecation, but must be manually reduced.
- Grade IV: The hemorrhoids are prolapsed and cannot be manually reduced.
Symptoms:
Many anorectal problems, including fissures, fistulae, abscesses,
anal melanoma or irritation and itching, also called pruritus ani, have
similar symptoms and are incorrectly referred to as hemorrhoids.
Hemorrhoids are usually not dangerous or life threatening. In
most cases, hemorrhoidal symptoms will go away within a few days.
Although many people have hemorrhoids, and hemorrhoidal
radiation, not all experience symptoms. The most common symptom of
internal hemorrhoidal radiation is bright red blood covering the feces
(hematochezia), on toilet paper, and/or in the toilet bowl. However, an
internal hemorrhoid may protrude through the anus outside the body,
becoming irritated and painful. This is known as a protruding
hemorrhoid.
Symptoms of external hemorrhoids may include painful swelling or a
hard lump around the anus that results when a blood clot forms. This
condition is known as a thrombosed external hemorrhoid.
In addition, excessive straining, rubbing, or cleaning around the
anus may cause irritation with bleeding and/or itching, which may
produce a vicious circle of symptoms. Draining anal mucus, produced by
the dentate line may also cause itching.
Causes:
Sitting for long periods of time can start the hemorrhoidic process.
Increased straining during bowel movements caused by constipation
or diarrhea may lead to hemorrhoids. It is thus a common condition due
to constipation caused by water retention in women experiencing
premenstrual syndrome or menstruation.
Hypertension, particularly portal hypertension, can also cause
hemorrhoids because of the connections between the portal vein and the
vena cava which occur in the rectal wall - known as portocaval
anastomoses.
Obesity can be a factor by increasing rectal vein pressure. Poor
muscle tone or poor posture can result in too much pressure on the
rectal veins.
Pregnancy may lead to hypertension and increase strain during
bowel movements, so hemorrhoids are often associated with pregnancy.
Insufficient liquid can cause a hard stool, or even chronic
constipation, which can lead to hemorrhoidal radiation. An excess of
lactic acid in the stool, a product of excessive consumption of dairy
products, such as yogurt, can cause radiation; reducing such consumption
can bring relief. Vitamin E deficiency is also a common cause. Eating
spicy food does not cause hemorrhoids, though spicy foods may aggravate
the condition.
Prevention:
Prevention of hemorrhoids includes drinking more fluids, eating
more dietary fiber (such as fruits, vegetables and cereals high in
fiber), exercising, practicing better posture, and reducing bowel
movement strain and time. Wearing tight clothing and underwear may also
contribute to irritation and poor muscle tone in the region and promote
hemorrhoid development.
Women who notice they have painful stools around the time of
menstruation would be well-advised to begin taking extra dietary fiber
and fluids a couple days prior to that time.
Fluids emitted by the intestinal tract may contain irritants that
may increase the fissures associated with hemorrhoids. Washing the anus
with cool water and soap may reduce the swelling and increase blood
supply for quicker healing and may remove irritating fluid.
Many people do not get a sufficient supply of dietary fiber (20
to 25 grams daily), and small changes in a person's daily diet can help
tremendously in both prevention and treatment of hemorrhoids.
Examination:
Endoscopic image of internal hemorrhoids seen on retro flexion of the flexible sigmoidoscope at the ano-rectal junction
After visual examination of the anus and surrounding area for
external or prolapsed hemorrhoids, a doctor may conduct a digital
examination. In addition to probing for hemorrhoidal bulges, a doctor
may also look for indications of rectal tumor or polyp, enlarged
prostate and abscesses.
Visual confirmation of hemorrhoids can be done by doing an
anoscopy, using a medical device called an anoscope. This device is
basically a hollow tube with a light attached at one end that allows the
doctor to see the internal hemorrhoids, as well as polyps in the
rectum.
If warranted, more detailed examinations, such as sigmoidoscopy
and colonoscopy can be performed. In sigmoidoscopy, the last 60 cm of
the colon and rectum are examined whereas in colonoscopy the entire
large bowel (colon) is examined.
Treatments:
Treatments for hemorrhoids vary in their cost, risk, and
effectiveness. Different cultures and individuals approach treatment
differently. Some of the treatments used are listed here in increasing
order of intrusiveness and cost.
Home treatments:
For many people, hemorrhoids are mild and temporary conditions
that heal spontaneously or by the same measures recommended for
prevention.
Temporary relief from symptoms can be provided by:
- Hydrotherapy with a bathtub, bidet, or extend-able shower
head. Especially in the case of external hemorrhoids with a visible lump
of small size, the condition can be improved with warm bath causing the
vessels around the rectal region to be relaxed.
- Cold compress.
- Topical analgesic (pain reliever), such as xylocaine or pramocaine.
- Systemic (pill-form) analgesic (pain reliever).
- Topical corticosteroid such as hydrocortisone. (May weaken the skin and may contribute to further flare-ups).
- Topical vasoconstrictor such as phenylephrine.
- Topical moisturizer.
Topical medicines may be delivered as an ointment or suppository.
Some hemorrhoid-specific medications contain a mixture of multiple
ingredients, such as Preparation H, Proctosedyl, and Faktu.
Ayurvedic Kshar-sutra application:
These days Ayurvedic Kshar-sutra treatment is in trends. This is
the method of treatment of hemorrhoids which is described in ancient
Ayurvedic grantha. It is showing high successful rate and negligible
reoccurrence. This is non surgical treatment and can be done by
experienced physician. In this treatment Kshar-sutra is applied in the
hemorrhoids under local anesthesia/general anesthesia and the pile mass
sheds off within seven to ten days with stool. Indian Council of Medical
Research (ICMR) has tried this technique in Hospitals in Metro Cities
for ten years and then declared this technique the most successful
procedure for treatment of hemorrhoids. In fistula in ano Kshar-sutra is
showing tremendous results. Most surgeons are also treating fistula in
ano with Kshar-sutra because surgery can cause incontinence and some
chances of reoccurrence are always there after surgery.
Surgical and Non-medicinal Treatments:
- Rubber band ligation, sometimes called Baron
ligation. Elastic bands are applied onto an internal hemorrhoid to cut
off its blood supply. Within several days, the withered hemorrhoid is
sloughed off during normal bowel movement.
- Hemorrhoidolysis, desiccation of the hemorrhoid by electrical current.
- Sclerotherapy, sclerosant or another hardening agent
is injected into hemorrhoids. This causes the vein walls to collapse and
the hemorrhoids to shrivel up.
- Cryosurgery, a frozen tip of a cryoprobe is used to destroy hemorrhoidal tissues. Rarely used anymore because of side effects.
- Hemorrhoidectomy, a surgical excision of the
hemorrhoid. Has possible correlation with incontinence issues later in
life; in addition, many patients complain that pain during recovery is
severe. For this reason it is often now recommended only for severe
(grade IV) hemorrhoids.
- Doppler guided hemorrhoidal artery ligation, which
cuts the artery that delivers blood to the hemorrhoid. It is the best
treatment for bleeding piles, as the bleeding stops immediately.
Natural Treatments:
- Eating fiber-rich diets, including water, helps create a
softer stool that is easier to pass, to lessen the irritation of
existing hemorrhoids.
- Using the squatting position for bowel movements.
- Dietary supplements can help treat and prevent many complications of hemorrhoids.
Diseases with Similar Symptoms:
Symptoms associated with rectal cancer, anal fissure, anal
abscess, anal fistula, perianal hematoma, and other diseases may be
similar to those produced by hemorrhoids and may be reduced by the
topical analgesic methods described above. For this reason, it is a good
idea to consult with a physician when these symptoms are encountered,
particularly for the first time, and periodically should the problem
continue. Colonoscopy is recommended as a general diagnostic for those
over age 50 (40 with family history of bowel cancers.
 Perianal
hematoma is caused by the rupture of a small vein that drains blood
from the anus. This rupture may be caused by heavy lifting, coughing,
straining, or bicycle riding. Once the rupture has formed, blood quickly
pools within a few hours and, if left untreated, forms a clot.
Perianal
hematoma is caused by the rupture of a small vein that drains blood
from the anus. This rupture may be caused by heavy lifting, coughing,
straining, or bicycle riding. Once the rupture has formed, blood quickly
pools within a few hours and, if left untreated, forms a clot.